Summer workshop student, Vedant Madabushi, interviews Alexander Honakala, an immunologist and researcher at Stanford University
Cancer is becoming a bigger threat to humanity – the National Institutes of Health (NIH) expects that by 2040, cancer diagnoses and deaths in the United States will rise to 29.5 million and 16.4 million individuals, respectively. The financial toll it has taken on healthcare is even worse. US cancer care spending in 2020 was around 210 billion dollars (NIH) and is expected to rise due to an aging population and the subsequent rise in cases. Fortunately, new approaches, methods, and technologies are being developed to combat the increasingly complex ways that tumors affect the human body.
I recently attended a genomics research summer workshop focused on Personalized Medicine, Big Data, and AI, conducted by the Department of Genetics at Stanford Medicine. One of the lectures was delivered by Alexander Honkala (Xander), a researcher from the Stanford Healthcare Innovation Lab. He has invested a lot of work into an up-and-coming field in oncology and has also founded Arxeon Therapeutics, a company based on this revolutionary science – cancer immunotherapy. This technique enables the immune system to fight cancer and holds immense potential for humanity.
I interviewed Xander as my final project for the workshop and gathered some excellent insights and takeaways: Before we move on, I strongly recommend viewing the interview in its entirety to gain a full perspective, in addition to the highlights captured below.
- Cancer immunotherapy as a field involves manipulating the microbiome of tumor cells in a way that the immune system is able to activate itself, a process known as immune modulation, and respond to a threat that usually breaks most pathogenic (bacterial and viral) norms. While our immune system does have a natural response to cancer cells, it has limited capabilities. Immunotherapy is able to effectively strengthen this response.
- Currently, most cancers cannot be cured through a single approach, but this can potentially change through immunotherapy. Due to the high rate of genetic mutations that occur with each cell division, cancer cells can differ between any two patients, or even within a single tumor. This leads to many issues in using mass-market drugs in cancer treatment, such as nonspecificity in treatment. These drugs also have varied negative effects on natural immune responses due to their dose-dependency – the amount of medicine administered in a single dose – and may increase overall resistance in cancer cells. This issue is addressed by assessing the differences between normal and cancer cells, focusing on individual cases’ unique needs and differences, while not generalizing treatment.
- Immunotherapy is also seeing great promise in treating diseases, such as Parkinson’s and Multiple Sclerosis because of the differences even within the same patient, like the types of cells affected. They may greatly benefit from immune modulation, a process in which the immune system activates itself.
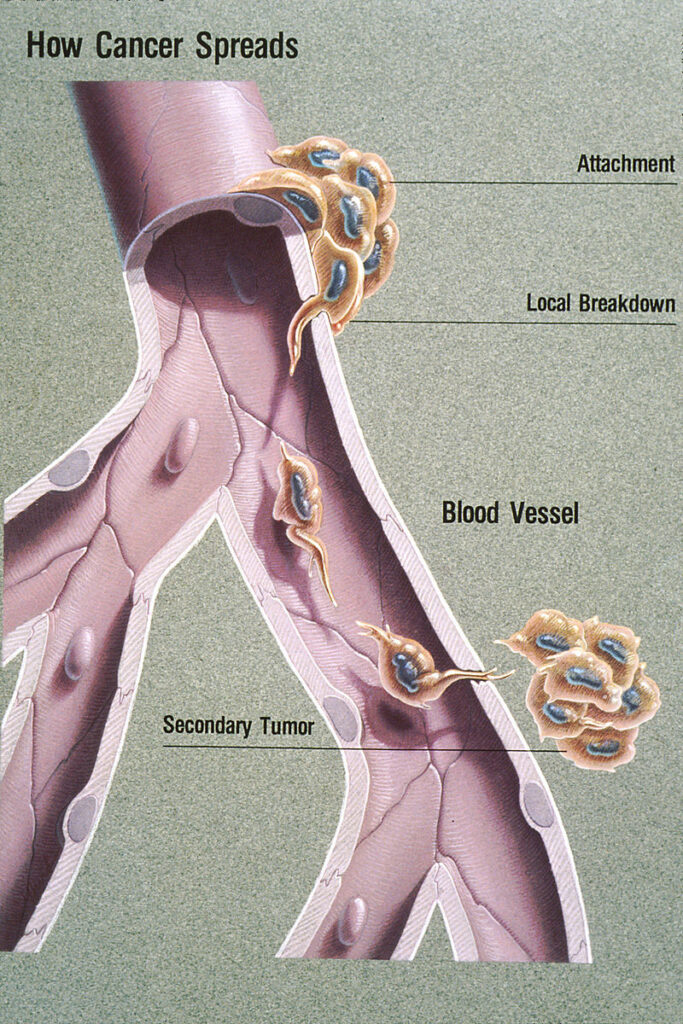
- The future of cancer immunotherapy is based mainly on currently developing drugs, including those that inhibit cancer cell cycles, which refers to the process cells grow, copy genetic material, and divide. Another application of immunotherapy, macrophage conditioning, may allow for the immune system’s white blood cells to more effectively recognize metastasizing cells well before they become a threat. Metastasis refers to the process through which cancer spreads to the rest of the body.
- Omics, the study of data that comes from different areas of an individual’s biological profile, is becoming more relevant to cancer immunotherapy, as the idea of personalized medicine becomes more widespread. For example, the differences in cells at particular locations of a tumor can be identified by analyzing their genomes. This data can further be used to develop treatment plans for individual patients. Proteins, RNA, and metabolites (chemicals used/produced in metabolic processes) can be analyzed in a similar manner. The massive amounts of data collected are not humanly possible to be analyzed manually. These datasets can be utilized to train machine learning models that can be inferred to assist healthcare professionals in diagnoses and improve patient outcomes.
- When any research projects of yours hit a dead end of any kind, learn when to stop pursuing it even if an emotional attachment has been formed. Forgo any losses that may potentially arise if the project starts to see diminishing returns. Then, make sure to look back on the project to see whether it is worth the time investment. At last, carry forward the lessons learned, and best practices into future projects.
- For students looking to enter immunology, develop a system for taking notes that is online and unique to your learning style. This allows you to log information in a format that can easily be comprehended and saved for later use. These notes also allow you to create mental models that you can apply the material to for an easier understanding.
Concluding Remarks
Before going into this interview, I knew I wanted to pursue a career in the life sciences and possibly immunology, but I could not entirely put my finger on a specific area of focus. Learning about Xander’s passionate stance on immunotherapy and the breakthroughs in developing mRNA COVID vaccines have ignited my interest to pursue a similar path. Immunotherapy encompasses the principles of oncology and computational work. I’m excited to learn more about the topics that Xander brought up in our conversation, such as macrophage conditioning and omics analysis, as well as utilizing immunotherapy and machine learning to diagnose, and treat diseases that hurt people’s well-being.
Biometrics, data collected from biological measurements specific to an individual, are soon to become more of a useful tool for healthcare professionals as personalized medicine is taking the front and center stage in all facets of the medical field. The health insights that will arise from this field will help form a healthcare system, where each patient’s needs are understood and prioritized.
While this is my first time interviewing a healthcare professional, I am thankful for what I have learned. My next steps are to explore and gain experience in AI, ML, and computational research in the field of immunology. I look forward to beginning this journey as a rising immunologist!
If you are interested in learning more about Xander’s work, this link is a great place to start.
Vedant Madabushi is a senior at Mission San Jose High School in Fremont, California. He got into biomedicine through a 7th-grade biology teacher, who lent him a copy of the medical textbook, Gray’s Anatomy. During the AP Biology class he took his junior year, he was first introduced to the idea of studying immunology and virology and developed his passion for it rapidly. Knowing that he’d have an opportunity to publish his work in a professional setting for the first time was inspiring and motivating. Bringing it to fruition has been a dream come true for him.
As we got to know Vedant while working with him, we learned a fun fact that he loves all kinds of spicy vegetarian food, and is up for the challenge to build to a higher tolerance. He would like to try Korean food. If you know a good Korean restaurant in the San Jose area that has vegetarian options, please send it our way to add to Vedant’s bucket list!