A Swift Response to Crisis

On December 12th, 2019, a group of patients in the city of Wuhan came down with pneumonia-like symptoms that did not improve with standard treatments. By January 3, 2020, the cases were reported to the World Health Organization (WHO), and a week later a draft genome was sequenced and published by the Global Initiative on Sharing All Influenza Data (GISAID). Less than a year later on December 11, 2020, the FDA made the Pfizer-BioNTech COVID-19 Vaccine available for patients 16 and older. The rapid development of the COVID-19 vaccine was an incredible success on behalf of the scientific and medical community, representing decades of research and design surrounding vaccines. Yet, some viewed the quick turnaround as a sign of hastiness and cutting corners. In this article, we will explore the development of the COVID-19 vaccine and understand where these misconceptions came from.
Past Vaccine Development
The historical development of vaccines, dating back to 1796 and the smallpox vaccine, has been a lengthy and complex process, but it led to significant advancements leading up to the COVID-19 vaccine. COVID-19, caused by the SARS-CoV-2 virus, is just one member of the larger coronavirus family. Coronaviruses are a group of related viruses that cause diseases in mammals and birds, and they are named for the crown-like spikes that protrude from their surfaces, resembling the sun’s corona. In humans, coronaviruses cause respiratory tract infections that can range from mild, like the common cold, to lethal, such as COVID-19.
June Almeida discovered the first coronavirus in the 1960s, yet the earnest quest for a coronavirus vaccine began after the outbreak of Severe Acute Respiratory Syndrome (SARS) in 2002 and Middle East Respiratory Syndrome (MERS) in 2012. These are both caused by coronaviruses, which are enveloped viruses with a crown-like appearance due to the spike proteins on their surface. The challenge for scientists was to find a way to stimulate the immune system to recognize and combat these viruses without causing disease. For SARS, the disease disappeared as suddenly as it appeared, and so the urgency to develop a vaccine decreased. For MERS, vaccine development faced challenges due to limited outbreaks, as well as the disease primarily affecting camels. However, despite these roadblocks, we gained substantial knowledge about coronaviruses, their spike proteins, and how they can be targeted to develop effective vaccines. Scientists conducted invaluable research that would eventually lead to the fast development of the COVID-19 vaccine.
Collaboration and Funding
The accelerated production of the COVID-19 vaccines can be largely attributed to unprecedented levels of collaboration across nations, sectors, and disciplines. While scientific discovery and innovative technologies played crucial roles, the collective effort and synergy across various fronts cannot be understated. Firstly, the rapid genomic sequencing and public sharing of the SARS-CoV-2 virus by Chinese scientists in January 2020 provided a foundational step. This shared knowledge allowed researchers worldwide to begin working on potential vaccines almost immediately. Multinational collaborations, such as the Coalition for Epidemic Preparedness Innovations (CEPI), further accelerated vaccine development by providing funding and bringing together expertise from academic institutions, industry, and public health bodies.

Next, pharmaceutical companies, typically competitors, embarked on uncommon partnerships. A prime example is the Pfizer-BioNTech alliance, which combined Pfizer’s global pharmaceutical experience with BioNTech’s expertise in mRNA technology. Simultaneously, Moderna collaborated closely with the National Institute of Allergy and Infectious Diseases (NIAID) in the United States, underscoring the vital partnership between public institutions and private companies. Johnson & Johnson and Merck, traditionally competitors in the pharmaceutical space, joined forces to increase the production capacity of the J&J single-dose vaccine under the US government’s direction.
The exceptional level of funding was another critical factor. This financial backing allowed companies to manufacture vaccines at risk – meaning, even before they had been approved. Normally, companies would wait for regulatory approval before investing in large-scale production. However, in this case, the urgent need for vaccines led to this extraordinary step, ensuring that millions of doses were ready for distribution as soon as approval was granted.
The massive scale and complexity of distributing COVID-19 vaccines posed another problem but is another example of widespread collaboration among governments, health organizations, private companies, and NGOs. Crucially, COVAX, an initiative co-led by CEPI, Gavi, and the WHO, facilitated global distribution to ensure equitable vaccine access. Domestically, partnerships between governments, logistics firms, and tech companies were crucial in handling the transportation, storage, and tracking of millions of doses. This collective effort, encompassing international alliances and domestic coordination, helped surmount the logistical challenges of delivering vaccines across the world.
Scientific Innovation
Many types of vaccines have been used in the past, such as inactivated, attenuated, and subunit vaccines. All of these vaccines work by taking the pathogen, whether in a dead or weakened (attenuated) form or small parts of it (subunit), and introducing it to the immune system so it can recognize the structure and build antibodies to fight it later on. While this approach has been around for decades, used to protect against influenza, polio, measles, mumps, and more, it has its drawbacks. To create the vaccine, the actual virus must be grown in a lab, which takes time and is costly to maintain. There is also the danger of non-virulent organisms converting into virulent organisms, or the body having a strong immune reaction to the pathogen, causing illness in the patient.

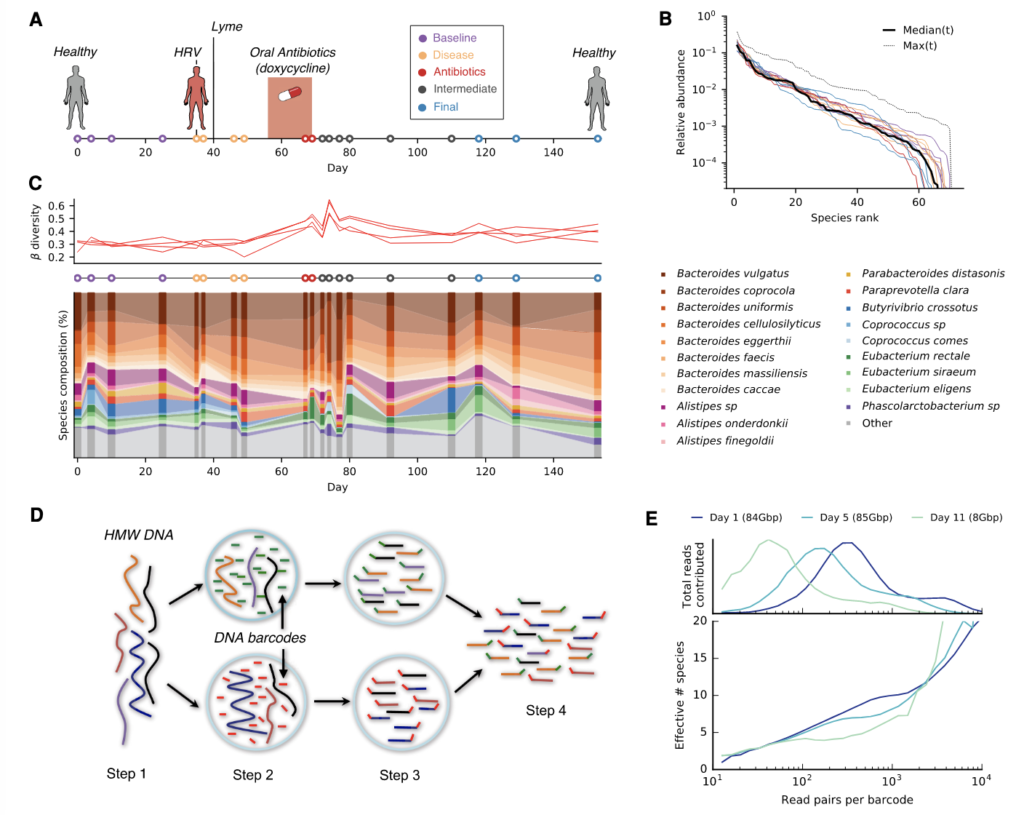
The two major vaccines distributed for COVID-19, created by Pfizer-BioNTech and Moderna, represented a breakthrough with the first approved mRNA vaccines. As the name suggests, these vaccines utilize mRNA, or messenger RNA to build up the body’s defenses. Instead of injecting a part of the pathogen, mRNA contains the instructions for the body to create the spike protein that gives COVID-19 its signature look. This protein then helps train the immune system, and when COVID-19 is introduced it can recognize the protein, and destroy it. This process mirrors the way human cells produce proteins, with mRNA acting as the intermediary between DNA and the cell’s protein-making ribosomes. Unlike the cell cultures required for traditional vaccines, mRNA vaccines are made of chains of macromolecules that can be manufactured much faster and more efficiently.
While this method has been in development for years, the COVID-19 pandemic marked the first time mRNA technology has been used in an authorized and widely distributed vaccine. The relative speed of designing and producing these vaccines, compared to traditional vaccine development timelines, underscored their potential in responding to future, novel pandemics. In addition, the mRNA platform offers flexibility, as it can be easily adjusted to target new strains of a virus, providing a dynamic tool against the evolving threat of infectious diseases. These vaccines, with their high efficacy and strong safety profiles, have set a new precedent for vaccine development, providing us with a powerful tool to combat future pandemics.
Clinical Trials
At each step of scientific development, the vaccine went through rigorous testing in clinical trials, assessing its safety and efficacy. Due to the urgent nature of the pandemic, researchers were able to enroll participants for the COVID-19 vaccine trials quickly. It was also crucial that these trials include participants from diverse backgrounds, ages, and health statuses to ensure the vaccine’s broad applicability. Many vaccine developers aimed for and achieved a racially and ethnically diverse group of participants, as well as representation from groups at higher risk for COVID-19, such as older adults and those with underlying health conditions.
While the rapid development of the COVID-19 vaccines was unprecedented, no steps were skipped in the safety monitoring of the trials. Safety data were continuously reviewed by external boards, known as Data and Safety Monitoring Boards (DSMBs). Furthermore, after the Emergency Use Authorizations (EUAs) were issued, safety monitoring systems were in place to detect potential side effects in the general population, including the Vaccine Adverse Event Reporting System (VAERS) and the CDC’s v-safe system, which allowed vaccine recipients to report side effects via their smartphones. As results from phase 3 trials emerged, many vaccines showed high levels of efficacy. For instance, Pfizer-BioNTech and Moderna vaccines, demonstrated around 95% and 94% efficacy, respectively. Based on this data, and with the DSMBs’ go-ahead, these companies applied for EUAs from the FDA, which were subsequently granted.

Vaccine Hesitancy
While the accelerated production of COVID-19 vaccines was a scientific triumph, it also became a source of concern for some individuals who feared the process was rushed at the expense of safety and thoroughness. Questions were raised as to whether all potential side effects could be known, given the relatively short testing and observation period. These claims were mostly unfounded, as, despite the accelerated timeline, no steps were skipped in the trial phases. Regulatory authorities globally maintained rigorous safety standards, and the vaccines were authorized only after an extensive review of their safety and efficacy data.

Compounding these fears was the spread of misinformation, often through social media platforms. False narratives, ranging from conspiracy theories about microchip implantation to unfounded claims about severe side effects, proliferated widely, sowing doubt and confusion. Some misinformation even propagated incorrect notions that the disease itself was a hoax, further discouraging vaccination. Efforts to debunk these myths often struggled to keep pace with the speed at which they spread.
Cultural, political, and ideological factors also played a role in vaccine hesitancy. For instance, some groups harbored historical mistrust in medical institutions due to past unethical practices, such as the Tuskegee syphilis study, making them more susceptible to misinformation and more hesitant to receive the vaccine. In some cases, vaccination became a politically polarizing issue, with attitudes towards it becoming entwined with personal and group identities, further complicating public health efforts.
Overcoming this hesitancy has required a multifaceted approach. This includes transparent communication about the development process and potential side effects, tailored outreach to specific communities, and interventions to limit the spread of health misinformation online. During the pandemic, many social media sites started reviewing their content for misinformation on COVID-19, and flagging those potential sources. Improving vaccination rates also involves amplifying the voices of trusted figures – from healthcare providers to community leaders – who can vouch for the vaccines’ safety and efficacy. Achieving widespread vaccination is not merely a scientific challenge, but also a test of our ability to effectively communicate scientific developments, combat misinformation, and foster trust in public health initiatives. It shows the reciprocal relationship between science and society, and how important it is to invest in science communication. Despite all of the hurdles, as of May 2023, 80% of the US has received at least one dose, and 70% are fully vaccinated.
Conclusion
The rapid development and distribution of COVID-19 vaccines stand as a beacon of what can be achieved when the world unites to combat a common enemy. Guided by scientific innovation, underpinned by extraordinary levels of global collaboration, and fueled by an urgency dictated by the pandemic, the vaccine rollout broke all previous records, marking a turning point in the annals of medicine and public health. The COVID-19 vaccines’ swift creation and distribution provide a roadmap for potential future challenges. The lessons learned, from the power of novel technologies like mRNA to the necessity of international cooperation, and the importance of managing public sentiment and combating misinformation will undoubtedly shape the future of global health. While we continue to navigate the complexities of the COVID-19 pandemic, the story of these vaccines serves as a powerful testament to human resilience, ingenuity, and the unwavering pursuit of protecting global health.
Adam Zaidi is a senior at San Francisco University High School. He is interested in the future of bioinformatics and bioengineering, and how technological advancements can be harnessed to improve the human condition. In addition, Adam is also concerned with bioethics, and engaging the human side in issues such as gender-affirming care are transhumanism. Outside of science, Adam enjoys playing jazz, word games, and making origami.